
DRY EYE
LEARN MORE ABOUT DRY EYE
Are you frustrated with how your eyes feel? Do you want answers and results? You're in the right place.

Do You Have Dry Eye?
Dry eye presents differently in every patient; therefore we take an individualized approach to your care. You may have dry eye if you experience:
Dryness, Grittiness, Scratchiness, Irritation, or Foreign Body Sensation
Excessive Tearing, Crusting or Debris, Redness, Styes, Irritated eyelids
Worsening or Fluctuating Vision, Frequent Prescription Changes, Intolerance to Contacts
Glare, Sensitivity to Light, Eye Fatigue, Headaches, or Double Vision (That Does Not Improve When Covering One Eye)
What To Expect At Your Dry Eye Evaluation
Your one hour long dry eye evaluation will start with a comprehensive history. You will be asked to fill out a questionnaire about your symptoms, lifestyle, medical history and medications, diet, and previous therapies. We use this information to coach you on changes you can make during your daily life to improve your symptoms. We discuss what has worked for you, and what has not, to avoid recreating the wheel.
We will then perform a series of tests to identify other underlying causes such as ocular inflammation, poor tear production, incomplete lid closure, allergies, mites or bacteria, clogged oil glands, low omega levels, tear evaporation, and more.
We wrap up the appointment by reviewing your results and connecting the dots between your causes and symptoms. We outline a treatment plan and discuss how each treatment works, how long it takes to be effective, and any potential side effects. You will be given samples, products, and a treatment guide with instructions leaving you feeling empowered to tackle your dry eye.

.avif)
What Is Dry Eye?
"Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles" as defined by the DEWS 2.
There are three layers to the tear film: Mucin, Aqueous, and Lipid. The bottom mucin layer is secreted by cells in the conjunctiva, and acts to keep tears on the eye. The middle aqueous layer is secreted by the lacrimal gland, and is the bulk of the tear film. The top lipid layer is secreted by meibomian glands in the eyelid to prevent the tears from evaporating.
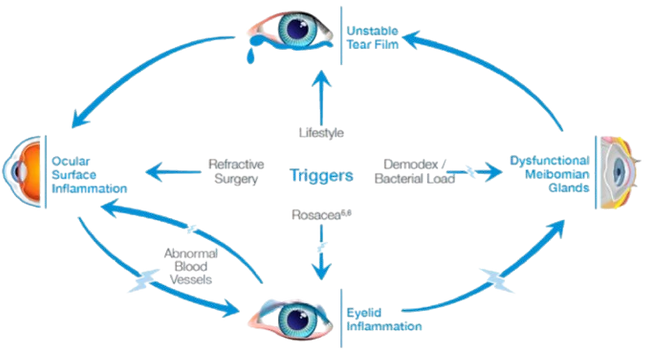
There are many reasons that the tear film can become dysfunctional, causing dryness of the ocular surface. Damaged tissue releases inflammation which causes more tissue damage, and the cycle worsens. For this reason, we classify dry eye as a chronic inflammatory condition.
My Dry Eye Philosophy

STEP ONE
Under Lying Cause
First and foremost, we treat the underlying cause of your dry eye. Whether it be low omegas, poor tear production, incomplete lid closure, mites in the eyelashes, or an autoimmune disease, we treat the problem at the source.
STEP TWO
Inflammation
Dry eye is an inflammatory condition that is chronic and progressive. We must control the underlying inflammation in order to successfully treat dry eye. There are many aways to control inflammation and many of which are prescription eye drops.

STEP THREE
Tissue Damage
Symptoms of dry eye stem from the tissue damage on the ocular surface. While we love to help patient's feel better quickly, many times we must wait to treat tissue damage until the underlying cause(s) and inflammation are controlled in order to get the best benefit. We do not want uncontrolled causes and inflammation to cause tissue damange to recur.

STEP FOUR
Nerve Damage
There are many reasons to have corneal nerve damage as a dry eye patient, including history of surgery, contact lens wear, and untreated dryness. In cases where the corneal nerves are damaged, such as neurotrophic keratitis, there the eye will not be able to heal itself unless we help regenerate the corneal nerves.
No two dry eye patients are the same, and therefore we provide every patient with an individualized dry eye treatment plan. It is important to understand that there is no one quick fix for dry eye, but a series of steps to provide the best results
Common Causes of Dry Eye
Find The Root Cause
Dry Eye is a multifactorial condition, which is why we perform an extensive evaluation to determine what is causing your symptoms. This allows us to treat the problem at the source. The list below is not exhaustive.

Meibomian Gland Dysfunction
The Meibomian Glands secrete the top layer of the tear film. Meibomian gland dysfunction, or MGD accounts for 86% of Dry Eye Cases.

Demodex Blepharitis
Demodex mites live in our lash follicles and can get out of control, causing dry eye symptoms.

Low Blood Omega Levels
The top layer of the tear film is lipid based, and requires normal omega blood levels to function properly. We check your omegas to ensure you are treating the problem at the source.

Low Tear Production
Low tear production requires very specific dry eye treatments. Testing to measure tear production, called shirmers, is vital to determine the underyling cause of your dry eye.

Systemic Conditions
Many systemic conditions can impact dry eye. Sjogrens, Thyroid Disorders, Diabetes, and Sleep Apnea are among the most common.

Medications
Many medications reduce tear production and can contribute to dry eye symptoms. We work with your other providers to ensure your systemic and ocular symptosm are controlled.

Incomplete Blink
The act of blinking releases oil from the meibomian glands in the eyelid. Digital technology and contact lens use reduces our blink rate and completeness, causing poor oil in the tear film, leading to tears evaporating too quickly.

Rosacea
Rosacea causes blood vessels from the face to feed inflammation to the eyelids and tear film. We offer the only FDA approved light therpy for this type of dry eye in Harford County.

Allergies
Allergies may be related to environment or even the eye drops you use for dry eye. We look at the big picture to make the link and address all underlying issues.
_edited.jpg)
Hormones
Tear production is regulated by hormones. It is important to treat dry eye but should not ignore systemic links. We work with other providers to help you feel better as a whole person.

Surgical
Surgeries such as LASIK, PRK, RK, and cataract surgery can contribute to dry eye by damaging corneal nerves that regulate tear production and tissue healing.

Contact Lens Wear
Chronic contact lens wear can cause dryness, loss of stem cells that regenerate the corneal surface, and reduce corneal nerve sensitivity, leading to poor healing.
Before and After
Real McConkey Eye Care Patients
Before treatment, patients experienced discomfort and blurred vision. The green in the photos is the tear film and staining of small abrasions and corneal tissue damage. The after photos will show much less staining, therefore symptom relief.
SOME KIND WORDS
Dr. McConkey truly cares about her patients. I’ve never felt rushed at any appointment. Her and her team are always kind and personable. I would highly recommend Dr. McConkey to anyone with dry eyes.
KELLY M

The Act of Blinking Releases Tears
Resources
Treating dry eye can be challenging, but we are here to support you.
Dry Eye Treatments
The Lumenis OptiLight IPL (Intense Pulsed Light) is a non-invasive treatment designed to help manage and treat dry eye disease (DED), particularly when the underlying cause is meibomian gland dysfunction (MGD). MGD is a common condition where the meibomian glands in the eyelids do not produce enough oil (lipid) for the tear film, leading to evaporative dry eyes. The OptiLight IPL treatment uses pulses of light to improve the function of these glands and address dry eye symptoms.
Key Features of Lumenis OptiLight IPL:
Intense Pulsed Light (IPL) Technology:
The OptiLight system uses intense pulsed light, which delivers light energy in multiple wavelengths to the skin around the eyes.
The light energy is absorbed by the meibomian glands and helps to liquefy and clear blockages in these glands, improving their function and increasing the flow of the oil necessary for a healthy tear film.
Targeting Meibomian Gland Dysfunction (MGD):
The treatment is specifically effective in cases of MGD, a leading cause of dry eye disease, as it helps restore the function of the meibomian glands and reduce gland obstruction.
By improving the oil component of the tear film, it helps to stabilize the tear film, reduce evaporation, and alleviate symptoms like dryness, irritation, and burning.
Comfort and Safety:
The procedure is generally safe and well-tolerated, with mild discomfort during the treatment. A cooling gel is often applied to the skin to enhance comfort during the procedure.
The IPL treatment is also designed to minimize side effects, with few reports of complications when used by trained professionals.
Non-Surgical and Non-Invasive:
OptiLight IPL is a non-surgical, non-invasive procedure that does not require any incisions or injections. It involves applying light pulses to the skin on the lower eyelids, targeting the meibomian glands indirectly.
How Lumenis OptiLight IPL Works:
Light Energy Application:
During the treatment, a specialized handpiece is used to deliver pulses of light to the skin around the eyes, specifically the area of the eyelids where the meibomian glands are located.
Improves Meibomian Gland Function:
The light energy targets the meibomian glands and helps to break down the blockages in the glands, which can be caused by thickened oil. The heat and light work to soften the oil and help the glands expel it.
Improves Tear Film Quality:
As the meibomian glands become more functional, they begin to produce a healthier oil layer in the tear film. This helps to stabilize the tear film, reduce evaporative dry eye, and relieve symptoms associated with dry eye disease.
Stimulates Skin Rejuvenation:
IPL may also help stimulate collagen production and improve the health of the skin around the eyes. This contributes to overall skin rejuvenation and may improve the appearance of fine lines and wrinkles around the eye area.
Treatment Process:
Pre-Treatment:
Before the procedure, the eye area is typically cleaned and a cooling gel may be applied to protect the skin and enhance the light's effectiveness.
IPL Application:
The IPL handpiece is placed near the skin around the eyes, and pulses of light are delivered to the treatment area. The light is absorbed by the targeted tissues, including the meibomian glands.
Duration:
The procedure typically lasts around 15-20 minutes and can be done in a clinical setting by a trained professional, such as an ophthalmologist or optometrist.
Post-Treatment Care:
After the treatment, there is generally no downtime. Patients may experience mild redness or warmth in the treated area, but these side effects typically resolve quickly.
Some patients may be advised to continue with other forms of treatment for dry eye disease, such as lubricating eye drops or eyelid hygiene routines, to support the results.
Benefits of Lumenis OptiLight IPL:
Improves Meibomian Gland Function:
The primary benefit of OptiLight IPL is its ability to improve meibomian gland function, helping to restore proper oil production in the tear film and reducing symptoms of dry eye disease caused by MGD.
Non-Invasive:
Unlike surgeries or injections, IPL is a non-invasive, painless treatment that can be performed in a short amount of time with minimal discomfort.
Improves Dry Eye Symptoms:
Many patients report significant improvement in dry eye symptoms, including reduced dryness, irritation, burning, and discomfort, following a series of IPL treatments.
Long-Term Relief:
Although results vary, many patients experience long-lasting relief from dry eye symptoms, with improvement often lasting for several months.
Skin Benefits:
In addition to improving meibomian gland function, IPL can also have aesthetic benefits, such as reducing fine lines and improving skin texture around the eyes due to its collagen-stimulating properties.
Potential Side Effects:
While Lumenis OptiLight IPL is generally considered safe, there are some potential side effects to be aware of:
Mild Redness or Warmth: The skin around the eyes may feel warm or appear slightly red immediately after treatment, but this usually resolves quickly.
Temporary Swelling: Some patients may experience mild swelling around the eyes following treatment.
Light Sensitivity: IPL treatment can make the skin more sensitive to light, so patients are often advised to avoid direct sun exposure after the procedure.
Eye Sensitivity: Although rare, some patients may experience temporary discomfort in the eyes.
Treatment Schedule:
The number of treatments needed varies by individual. Typically, a series of 3-4 sessions is recommended, spaced 3-4 weeks apart for optimal results. Maintenance treatments may be suggested every 6-12 months, depending on the patient's needs and the severity of their dry eye disease.
Conclusion:
Lumenis OptiLight IPL is an innovative, non-invasive treatment for managing dry eye disease, especially when caused by meibomian gland dysfunction. By using intense pulsed light, it helps improve meibomian gland function, reduce inflammation, and restore proper oil production in the tear film, providing lasting relief from dry eye symptoms. With minimal downtime and relatively few side effects, it offers a promising option for patients who have not found relief with traditional treatments for dry eyes. Always consult with an eye care professional to determine if OptiLight IPL is right for your dry eye treatment plan.
Punctal plugs are a treatment option for people with aqueous deficient dry eye, a condition in which the eyes do not produce enough tears to keep the ocular surface properly lubricated. These plugs are small devices inserted into the puncta — the small openings on the eyelids that drain tears into the nasal cavity. By blocking or reducing the drainage of tears, punctal plugs help to retain more of the natural tears that are produced, offering relief from the dryness, irritation, and discomfort that come with dry eye disease.
There are two main types of punctal plugs used to treat aqueous deficient dry eye: silicone plugs and collagen plugs. Both types work to improve tear retention, but they have different materials, characteristics, and durations of effectiveness.
1. Silicone Punctal Plugs
Silicone plugs are a popular and commonly used type of punctal plug, particularly for those with chronic dry eye or aqueous deficient dry eye. These plugs are made of a flexible, durable silicone material that is designed to stay in place for a long time.
Key Features of Silicone Punctal Plugs:
Long-Term Solution: Silicone plugs are permanent (or semi-permanent) and typically do not need to be replaced often. Once inserted, they can stay in the punctum for months or even years, depending on the patient’s condition and the type of plug used.
Retention of Tears: Silicone punctal plugs are designed to block tear drainage more effectively, which helps to increase the amount of tear film available on the surface of the eye, providing long-lasting moisture and reducing symptoms of dry eye.
Customizable Fit: Silicone plugs come in various sizes and shapes, allowing for customization to fit the individual patient's anatomy and needs. Some plugs are designed to be adjustable, allowing for fine-tuning after insertion.
Permanent or Refillable: These plugs are generally designed to be permanent, though some are removable or may need to be adjusted over time. They are inserted by an eye care professional and can be removed if necessary.
Advantages:
Long-lasting relief from dry eye symptoms.
Minimal maintenance required.
Reduces the need for frequent artificial tear use.
Can be used in both lower and upper puncta (tear drainage openings).
Disadvantages:
Not suitable for all patients, especially those with punctal scarring or other anatomical issues.
In rare cases, the plug may cause irritation, infection, or become displaced.
OverpluggingOver plugging can cause excessive tearing
Procedure:
Silicone punctal plugs are usually inserted in an in-office procedure by an ophthalmologist or optometrist. The procedure involves inserting the plugs into the puncta using specialized instruments. Local anesthetic drops may be used to numb the area, ensuring the procedure is painless.
2. Collagen Punctal Plugs
Collagen punctal plugs are another type of punctal plug, made from a biodegradable collagen material. These plugs are typically used as a temporary solution for dry eye management, often for those who are new to punctal plugs or for those who want to test the effectiveness of the treatment before committing to permanent silicone plugs.
Key Features of Collagen Punctal Plugs:
Temporary Solution: Collagen plugs dissolve over time, usually within a few days to weeks. This makes them ideal for patients who want to test the efficacy of punctal plugs before opting for a more permanent solution like silicone plugs.
Less Durable: Since collagen plugs are designed to dissolve, they do not provide the long-term relief that silicone plugs offer. However, they can still help reduce dry eye symptoms for the duration they remain in place.
Biodegradable: The collagen material gradually breaks down and is absorbed by the body, meaning patients do not need to worry about the plugs needing removal. This makes them a low-maintenance option.
Reduced Risk of Overplugging: Because they are temporary, collagen plugs reduce the risk of complications like excessive tearing or discomfort from overplugging.
Advantages:
Temporary, offering a trial period to assess whether punctal plugs are effective.
Biodegradable, so no removal is necessary.
Minimal risk of side effects since they are designed to dissolve naturally.
Can be an ideal choice for patients who are uncertain about long-term treatment.
Disadvantages:
Short-term effectiveness, requiring replacement if long-term relief is desired.
May not be suitable for patients with severe dry eye who require long-lasting moisture retention.
Requires more frequent replacements compared to silicone plugs.
Procedure:
Like silicone plugs, collagen plugs are inserted by an eye care professional in an office setting. The process is similar, with the plugs being inserted into the puncta using specialized tools. Local anesthesia is typically used to ensure comfort during the procedure.
Choosing Between Silicone and Collagen Punctal Plugs:
The choice between silicone and collagen punctal plugs depends on the patient's specific condition, treatment goals, and preference:
Silicone Punctal Plugs:
Best for individuals with chronic dry eye or those who need long-term relief.
Ideal for patients who do not want frequent replacements.
Suitable for both lower and upper puncta.
Collagen Punctal Plugs:
Ideal for temporary relief or for patients who want to test the efficacy of punctal plugs.
Best for those who prefer a non-permanent solution or who have relatively mild dry eye.
More suitable for individuals who may want to evaluate the effect of punctal plugs without committing to a permanent solution.
Benefits of Punctal Plugs for Aqueous Deficient Dry Eye:
Increased Tear Retention: By blocking the puncta, these plugs reduce tear drainage, which helps retain more of the body’s own tears and increases moisture on the ocular surface.
Improved Comfort: Many patients with aqueous deficient dry eye report improved comfort and reduced symptoms of dryness, burning, and irritation after using punctal plugs.
Reduction in Artificial Tear Use: Punctal plugs can decrease the need for frequent use of artificial tears or other lubricating eye drops, leading to greater convenience.
Non-Invasive: The procedure is minimally invasive and is performed in-office without the need for surgery or lengthy recovery times.
Potential Risks and Side Effects:
Discomfort: Some patients may experience discomfort or a feeling of pressure after the insertion of punctal plugs, especially if the plugs do not fit properly.
Infection: Though rare, there is a slight risk of infection or inflammation at the site of insertion.
Displacement: The plugs may become displaced or fall out, especially if they are not securely fitted. This is more common with temporary collagen plugs.
Excessive Tearing: In rare cases, punctal plugs can cause excessive tearing (epiphora) if too many tears are trapped in the eye, leading to discomfort.
Allergic Reactions: Some individuals may have allergic reactions to the material of the plugs, although this is uncommon.
Conclusion:
Punctal plugs, whether silicone or collagen, are effective treatments for aqueous deficient dry eye, especially when meibomian gland dysfunction is the underlying cause. Silicone plugs provide long-term relief, while collagen plugs offer a temporary solution for testing effectiveness. Both options are minimally invasive and have proven to improve comfort and reduce symptoms associated with dry eye disease. Working with an eye care professional is essential in determining the best type of punctal plug and ensuring proper insertion and monitoring for optimal results.
Zest by Zocular is a lid hygiene and ocular health product designed to help manage and maintain the health of the eyelids and lashes, particularly for those suffering from dry eye disease, blepharitis, and meibomian gland dysfunction (MGD). It contains okra-based ingredients and is marketed as a gentle, natural solution for eyelid hygiene and maintaining the health of the eyelid and ocular surface.
Key Features of Zest by Zocular:
Okra-Based Formula:
Zest is formulated with okra extract, which is a natural ingredient known for its soothing, hydrating, and anti-inflammatory properties. Okra is rich in mucilage, a gel-like substance that helps moisturize and calm the eyelid area, and it is used for its potential ability to remove debris, reduce inflammation, and improve lubrication around the eyes.
Cleansing and Hygiene:
Zest provides a gentle, yet effective, eyelid cleanse, helping to remove dirt, oil, and debris from the eyelids and lashes. This is particularly important for individuals with conditions like blepharitis, where the eyelid margins may become inflamed due to bacteria, oils, or debris.
Supports Healthy Meibomian Glands:
By improving eyelid hygiene, Zest can help with meibomian gland dysfunction (MGD), a leading cause of evaporative dry eye. MGD occurs when the oil-producing glands in the eyelids become blocked, causing tears to evaporate too quickly and leading to dry eye symptoms. Keeping the eyelids clean and clear of debris supports proper meibomian gland function.
Soothing and Non-Irritating:
The okra extract in Zest is soothing and non-irritating, making it suitable for individuals with sensitive skin or eyes. It can provide relief from discomfort, itching, and inflammation around the eyes, which are common symptoms of dry eye disease or blepharitis.
Convenient and Easy to Use:
Zest is available in a foam or wipe format, making it easy to use as part of a daily eyelid hygiene routine. It can be applied directly to the eyelids and lashes, offering a simple way to maintain eyelid cleanliness and ocular health.
Benefits of Zest by Zocular:
Cleanses and Refreshes:
Zest helps to gently clean the eyelid area without harsh chemicals, alcohol, or preservatives. This gentle cleaning action helps reduce inflammation and irritation, keeping the eyelid and lash line clear of debris and oils that can contribute to dry eye symptoms.
Supports Tear Film Health:
By promoting a healthy eyelid environment, Zest can help improve the stability of the tear film, which is essential for maintaining moisture on the ocular surface. This is particularly beneficial for individuals with aqueous deficient dry eye or meibomian gland dysfunction (MGD), as a clean lid environment can aid in the proper functioning of the tear glands.
Reduces Symptoms of Blepharitis:
Zest is particularly useful for people with blepharitis, a condition where the eyelids become inflamed, often due to bacterial growth or blocked glands. By regularly cleaning the eyelids and removing bacteria or excess oils, Zest can help reduce symptoms like redness, swelling, itching, and discomfort.
Natural and Gentle:
With its natural okra-based ingredients, Zest is a gentler alternative to harsher cleaning products that may contain alcohol or preservatives, making it suitable for individuals with sensitive eyes or skin around the eyelids.
How to Use Zest by Zocular:
Foam:
Shake the bottle gently before use.
Apply a small amount of the foam to a clean cotton pad, gauze, or directly to the eyelids.
Gently massage the foam onto the eyelid area and the lash line, ensuring to remove any debris, oil, or dirt.
Rinse the area with lukewarm water or wipe with a clean tissue, if necessary.
Wipes:
If using the pre-moistened wipes, simply use one wipe to gently clean the eyelids and lashes.
Wipe along the eyelid margins and lash line to remove any buildup of oils or debris.
Discard the wipe after use.
Potential Side Effects and Considerations:
Minimal Irritation: Zest is generally well-tolerated and designed for sensitive skin around the eyes. However, if irritation or redness occurs, discontinue use and consult an eye care professional.
Contact Lenses: If you wear contact lenses, it’s advisable to remove them before using Zest, as the product may contain ingredients that could interact with your lenses.
Consistency: For optimal results, use Zest regularly as part of your daily eyelid hygiene routine. The product is usually recommended for daily use, and consistency is key to managing dry eye symptoms and maintaining healthy eyelids.
Conclusion:
Zest by Zocular is a gentle, okra-based eyelid treatment designed to support ocular health and dry eye management by improving eyelid hygiene and promoting the health of the tear film. It is particularly useful for individuals with meibomian gland dysfunction (MGD), blepharitis, and aqueous deficient dry eye, offering a natural, soothing alternative to harsher chemical-based eyelid treatments. By cleansing the eyelid area, reducing inflammation, and improving gland function, Zest can help alleviate symptoms of dry eyes and contribute to overall eye comfort.
Gland expression is a common and effective treatment for Meibomian Gland Dysfunction (MGD), a condition where the Meibomian glands in the eyelids fail to produce an adequate amount of oil (meibum) needed to form a stable tear film. This dysfunction leads to dry eye symptoms, irritation, and discomfort, as the tear film becomes unstable and evaporates too quickly.
What is Meibomian Gland Dysfunction (MGD)?
MGD occurs when the Meibomian glands, located in the upper and lower eyelids, become blocked or inflamed, preventing them from secreting the oil that helps lubricate and protect the surface of the eye. Without this oily layer, the tears evaporate too quickly, leading to dryness, itching, burning, redness, and even blurry vision.
The blockage can be caused by various factors, such as:
Inflammation of the glands
Thickened meibum (the oil produced by the glands)
Reduced blinking frequency
Hormonal changes
Aging
Environmental factors (dry air, wind)
What is Gland Expression?
Gland expression refers to the process of releasing the built-up oils (meibum) from the Meibomian glands to restore proper functioning. The procedure is performed by an eye care professional (optometrist or ophthalmologist) and aims to clear the blockages in the glands and improve oil production.
There are two main types of gland expression:
Manual Gland Expression:
This method involves the gentle manual expression of the Meibomian glands using pressure on the eyelids.
The eye care provider will typically use their fingers or a specialized tool to apply gentle pressure along the eyelids (near the lash line). This helps push the thickened oils out of the glands.
Manual expression is often done after warming the eyelids (using a warm compress or specialized device) to soften the meibum, making it easier to express the oils.
Thermal Pulsation Devices (e.g., LipiFlow):
Thermal pulsation systems, such as LipiFlow, are often used to treat MGD by combining heat and gentle pressure to open the Meibomian glands and help release the thickened oil.
These devices are FDA-approved and use controlled heat and pulsatile pressure to treat the glands without direct manual pressure. The heat softens the meibum, while the pulsatile pressure helps express the oils from the glands.
LipiFlow, for example, involves placing a device on the eyelids, which applies precise heat to the inner eyelids while also delivering gentle pressure to the glands.
Benefits of Gland Expression for MGD:
Improved Tear Film Stability:
By expressing the oils from the Meibomian glands, gland expression helps restore the lipid layer of the tear film, which reduces tear evaporation and improves eye lubrication. This results in relief from dry eye symptoms like burning, itching, and redness.
Relieves Symptoms of Dry Eye:
Gland expression can provide immediate relief from the discomfort associated with MGD by improving the oil flow to the surface of the eye and reducing inflammation in the eyelids.
Enhances Oil Production:
Regular gland expression can help stimulate the Meibomian glands and encourage healthier oil production. This can lead to long-term relief from dry eye symptoms and improve overall eye health.
Reduces Eye Inflammation:
Gland expression may help reduce inflammation around the glands and the eyelid area, which can further reduce symptoms like redness and swelling of the eyelids.
Quick and Non-Invasive:
Both manual gland expression and thermal pulsation treatments are non-invasive and relatively quick, with most treatments taking around 15-30 minutes. There is minimal discomfort involved, and the procedure is typically well-tolerated.
How Gland Expression Is Performed:
Preparation:
The process usually begins with a warm compress or the use of a specialized heat system (such as a heat mask) applied to the eyes to soften the meibum. This helps make the oil easier to express.
Expression:
In the case of manual expression, the provider will apply gentle pressure to your eyelid, either with their fingers or using a specialized tool designed for this purpose.
For thermal pulsation systems like LipiFlow, the device will be placed on the eyelids to deliver heat and pulsatile pressure, helping to express the oils from the glands.
Post-Procedure Care:
After the procedure, your provider may recommend lubricating drops to keep your eyes hydrated and soothe any mild discomfort.
Some individuals may experience mild tenderness or a feeling of fullness in the eyelids after the procedure, but these symptoms are typically short-lived.
Frequency of Gland Expression:
The frequency of gland expression can vary depending on the severity of MGD and the individual’s response to treatment. Typically, several sessions may be required over a period of weeks to achieve long-lasting results. Some patients may need maintenance treatments every few months, while others may only need periodic expression.
Your eye care professional will be able to recommend the best treatment plan based on the severity of your MGD and any underlying conditions.
Other Treatments to Complement Gland Expression:
Gland expression is often used in combination with other treatments to manage MGD effectively:
Warm compresses: Regular use of a warm compress helps soften the meibum and prevent future blockages.
Lid hygiene: Cleaning the eyelids regularly with lid scrubs or hypochlorous acid-based wipes can help remove debris and bacteria that contribute to MGD.
Omega-3 fatty acids: Supplements rich in omega-3s (such as fish oil) can help improve the quality of the oils produced by the Meibomian glands.
Anti-inflammatory medications: Medications such as cyclosporine A (Restasis) or lifitegrast (Xiidra) can reduce inflammation in the eyes.
Punctal plugs: If dry eye is severe, punctal plugs can be used to block the tear drainage ducts, helping retain moisture on the eye's surface.
Potential Side Effects of Gland Expression:
While gland expression is generally safe, some people may experience mild discomfort, redness, or irritation of the eyelids immediately after the procedure. These symptoms are typically temporary and should resolve quickly.
In rare cases, there may be pain or swelling of the eyelids, but this is uncommon. If any unusual symptoms occur, it is important to consult your eye care provider.
Conclusion:
Gland expression is a highly effective treatment for Meibomian Gland Dysfunction (MGD), helping to improve the flow of oils from the Meibomian glands, restore tear film stability, and alleviate the symptoms of dry eye. By combining gland expression with other management strategies like warm compresses, lid hygiene, and anti-inflammatory treatments, many individuals can find significant relief from their MGD symptoms and improve their eye comfort and health. Always consult with your eye care provider to determine the best treatment plan for your specific needs.
Scleral lenses are a highly effective treatment option for individuals with dry eye disease, particularly for those with severe or chronic dry eyes that are not easily managed with artificial tears or other conventional treatments. These lenses are large-diameter, gas permeable contact lenses that vault over the entire cornea and rest on the sclera (the white part of the eye), providing unique benefits for dry eye sufferers.
Here’s a breakdown of how scleral lenses work and why they are often used for treating dry eye disease:
How Scleral Lenses Help with Dry Eye:
Tear Reservoir:
One of the primary benefits of scleral lenses for dry eye treatment is that they create a tear reservoir between the lens and the cornea. The space between the lens and the cornea fills with saline solution or a lubricating solution, which provides constant hydration and protection to the corneal surface.
This helps to alleviate dryness and discomfort because the tear film is maintained throughout the day, reducing symptoms like dryness, burning, and irritation.
Protection of the Cornea:
Scleral lenses provide a protective barrier over the cornea, shielding it from the environment, allergens, and irritants that can exacerbate dry eye symptoms. For patients with ocular surface disease or damaged corneas, scleral lenses offer much-needed protection.
Stable Tear Film:
Dry eye is often caused by an unstable tear film, which leads to evaporation of tears and inadequate lubrication of the ocular surface. Scleral lenses help stabilize the tear film by reducing evaporation and maintaining moisture under the lens, ensuring more consistent hydration.
Relief for Aqueous Deficient Dry Eye:
Scleral lenses are particularly beneficial for people with aqueous deficient dry eye, where the eyes do not produce enough tears. The lens acts as a reservoir of fluid, supplying moisture to the eye even in the absence of sufficient natural tear production.
Meibomian Gland Dysfunction (MGD) Relief:
Meibomian gland dysfunction (MGD) is a leading cause of dry eye, where the oil-producing glands in the eyelids become blocked, leading to rapid evaporation of tears. Scleral lenses can help minimize tear evaporation and provide relief from the dryness caused by MGD by creating a sealed moisture environment on the eye surface.
Comfort for Severe Dry Eye:
Traditional contact lenses often worsen dry eye symptoms because they draw moisture away from the eye, leading to increased discomfort. In contrast, scleral lenses provide a consistent moisture supply, which can be extremely beneficial for individuals with severe or chronic dry eye conditions.
Types of Dry Eye Conditions Treated with Scleral Lenses:
Aqueous Deficient Dry Eye:
This type of dry eye is caused by an insufficient quantity of tears produced by the lacrimal glands. Scleral lenses help by creating a tear reservoir that hydrates the cornea, reducing symptoms of dryness and discomfort.
Meibomian Gland Dysfunction (MGD):
MGD occurs when the oil-producing glands in the eyelids become blocked or produce insufficient oil, leading to rapid evaporation of the tear film. Scleral lenses can help by stabilizing the tear film and preventing evaporation, offering relief from this condition.
Blepharitis:
This is inflammation of the eyelid margins, which can contribute to dry eye symptoms. Scleral lenses can protect the ocular surface and provide moisture, offering comfort to individuals with blepharitis.
Post-Surgical Dry Eye:
After certain eye surgeries, such as LASIK or cataract surgery, patients may experience dry eye. Scleral lenses can provide relief by creating a stable tear reservoir and protecting the healing cornea.
Keratoconus:
Scleral lenses are particularly effective for individuals with keratoconus, a condition where the cornea becomes thin and irregularly shaped. The lens creates a smooth optical surface and helps stabilize tear distribution, providing comfort and visual clarity.
Autoimmune Diseases:
Conditions like Sjogren’s syndrome can cause severe dry eye symptoms. Scleral lenses are often recommended for these patients to provide long-lasting hydration and comfort.
How Scleral Lenses Are Fitted:
Custom Fit:
Unlike standard contact lenses, scleral lenses are custom-designed for each patient’s eye. A detailed fitting process is necessary to ensure that the lens is the correct size and curvature to provide optimal comfort and vision. The fitting process includes measuring the corneal shape and scleral curvature using specialized equipment.
Tear Film Evaluation:
The eye care professional will also evaluate the tear film to ensure that the lens creates an adequate tear reservoir to keep the cornea hydrated. The lens should create a fluid layer between the lens and the eye, which is essential for alleviating dry eye symptoms.
Trial Lenses:
During the fitting process, trial lenses are used to assess comfort and the amount of tear film under the lens. Adjustments are made to ensure the lens provides the best fit and most effective moisture retention.
Benefits of Scleral Lenses for Dry Eye:
Long-Lasting Comfort:
Scleral lenses provide prolonged comfort throughout the day because they create a stable tear reservoir under the lens. For patients with severe dry eye, this consistent moisture is invaluable for relieving irritation and discomfort.
Improved Vision:
In addition to providing comfort, scleral lenses can improve vision, particularly for individuals with irregular corneas (e.g., keratoconus) or scarring caused by dry eye disease. The lens creates a smooth surface, improving optical clarity.
Protection from Environmental Irritants:
Scleral lenses shield the cornea from irritants like dust, smoke, or allergens, which can exacerbate dry eye symptoms. The lens also acts as a physical barrier to the environment, providing added protection for the eyes.
Reduction in the Need for Artificial Tears:
Many patients who use scleral lenses experience a reduced need for frequent use of artificial tears, as the lenses provide constant moisture to the eye. This can be particularly beneficial for patients who struggle with the high frequency of artificial tear instillation.
Improved Quality of Life:
For patients with severe dry eye, scleral lenses can dramatically improve quality of life by reducing discomfort and restoring normal vision. They are especially helpful for individuals who have not found sufficient relief with other treatments.
Potential Challenges:
Initial Fitting Process:
The fitting of scleral lenses can be more complex than regular contact lenses, requiring specialized expertise. Patients must work closely with an eye care professional to ensure an optimal fit.
Care and Maintenance:
Scleral lenses require proper cleaning, disinfection, and regular maintenance to ensure they remain safe and effective. Some patients may find this routine more demanding compared to traditional contact lenses.
Cost:
Scleral lenses can be more expensive than standard contact lenses, especially because they are custom-made and may require additional fittings and follow-up appointments. However, many patients find that the benefits in terms of comfort and symptom relief make the cost worthwhile.
Conclusion:
Scleral lenses are an excellent option for treating dry eye disease, especially for individuals with severe or chronic dry eyes that are caused by conditions like aqueous deficient dry eye, meibomian gland dysfunction, or autoimmune diseases. These lenses create a protective, moisture-retentive reservoir that keeps the cornea hydrated throughout the day, providing relief from dryness, irritation, and discomfort. Though they require a detailed fitting process and proper care, the benefits of scleral lenses for dry eye sufferers—such as long-lasting comfort, improved vision, and reduced dependency on artificial tears—make them a highly effective solution for managing dry eye symptoms.
Radiofrequency (RF) therapy is a relatively new and innovative treatment option for managing dry eye disease (DED), especially when it's associated with Meibomian Gland Dysfunction (MGD), one of the most common causes of dry eye. RF therapy uses targeted heat energy to treat the glands and improve tear film stability, providing relief from symptoms such as dryness, irritation, and discomfort.
What is Radiofrequency Therapy for Dry Eye?
Radiofrequency therapy for dry eye involves the application of radiofrequency energy (a form of electrical energy) to the eyelids and surrounding tissues. This energy generates heat that is used to warm the Meibomian glands and the eyelid tissues, aiming to melt thickened meibum (the oil produced by the glands) and stimulate better gland function. The primary goal is to improve the production and flow of the oils from the Meibomian glands to stabilize the tear film and reduce dry eye symptoms.
How Does Radiofrequency Therapy Work?
Targeting Meibomian Glands:
Radiofrequency therapy targets the Meibomian glands, which are responsible for producing the oily layer of the tear film. In people with MGD, the oil produced by these glands can become thickened or clogged, leading to decreased oil production and an unstable tear film. This instability leads to dryness and increased evaporation of tears.
Heat Application:
The device used in RF therapy applies gentle heat to the eyelids using radiofrequency waves. The heat helps melt thickened meibum, clearing blockages in the glands. The heat also stimulates the glands, which can lead to increased production of normal, less viscous oils.
Stimulation of Gland Function:
The RF energy helps to enhance the natural function of the Meibomian glands, promoting healthier and more efficient oil production. This reduces the likelihood of blockages and helps to restore the tear film's lipid layer, which reduces tear evaporation and improves overall eye lubrication.
Non-Invasive and Comfortable:
RF therapy is a non-invasive procedure that does not involve direct manipulation of the glands, unlike manual gland expression. The process is generally comfortable, with patients often reporting a warm sensation on their eyelids during the treatment.
Benefits of Radiofrequency Therapy for Dry Eye:
Improves Meibomian Gland Function:
RF therapy is particularly beneficial for people with Meibomian Gland Dysfunction (MGD), as it helps restore normal function to the glands, improves oil secretion, and enhances the overall tear film quality.
Reduces Dry Eye Symptoms:
By improving the quality and stability of the tear film, RF therapy can significantly reduce common dry eye symptoms such as dryness, itching, burning, and redness. The increased oil production helps reduce tear evaporation and provides better lubrication to the eye surface.
Stimulates Collagen Production:
Radiofrequency therapy can also stimulate collagen production in the eyelid tissues, which helps improve the structural integrity of the glands and surrounding tissues, potentially improving gland function over the long term.
Safe and Non-Surgical:
Unlike surgical options or invasive procedures, radiofrequency therapy is a non-surgical and non-invasive treatment that can be performed in an outpatient setting, making it a more accessible and less risky treatment option for those suffering from MGD-related dry eye.
Minimal Downtime:
There is minimal downtime after the procedure, with most patients experiencing little to no discomfort and being able to resume their normal activities immediately following treatment.
Long-Lasting Relief:
Many patients experience long-lasting improvement in symptoms following RF therapy, especially when combined with other dry eye treatments such as lid hygiene, lubricating eye drops, or omega-3 supplements.
The Procedure:
Pre-Treatment Preparation:
Before the procedure, your eye care provider will assess your dry eye condition and may recommend a lid hygiene regimen to prepare the eyelids. Some topical anesthetic drops may be applied to ensure comfort during the treatment.
Application of RF Energy:
A specialized RF device is gently placed over the closed eyelids. The device generates radiofrequency energy that is delivered to the eyelid tissues. The heat generated by this energy will typically feel warm, and the provider will adjust the temperature and intensity for optimal comfort and effectiveness.
Treatment Duration:
Each session typically lasts between 15 to 20 minutes, depending on the severity of the dry eye and the area being treated. The treatment is typically well-tolerated, with minimal discomfort.
Post-Treatment Care:
After treatment, you may be advised to apply lubricating eye drops to help soothe the eyes. It’s important to avoid rubbing the eyes for a short period after the treatment to prevent irritation.
Follow-up Treatments:
Depending on the severity of your MGD and dry eye, you may need multiple treatments to achieve the desired results. Your eye care professional will tailor the treatment plan based on your specific needs.
Side Effects and Considerations:
Mild Discomfort: Some patients may experience mild discomfort or warmth during the procedure, but these sensations are typically brief and well-tolerated.
Temporary Redness: After treatment, some people may notice mild redness or swelling of the eyelids, but this usually resolves quickly within a few hours.
Sensitivity: A few individuals may experience temporary sensitivity to light or some irritation following the procedure, but these side effects are generally short-lived.
Infection Risk: As with any eye treatment, it is important to follow aftercare instructions to reduce the risk of infection. However, RF therapy itself is low-risk when performed by a trained professional.
Conclusion:
Radiofrequency therapy is an effective, non-invasive treatment option for dry eye disease, particularly in cases where Meibomian Gland Dysfunction (MGD) is the primary cause. By applying gentle heat to the eyelid tissues, RF therapy helps unclog Meibomian glands, improve oil secretion, and restore tear film stability, leading to relief from common dry eye symptoms. It is a safe and well-tolerated treatment with minimal downtime and can be combined with other therapies for optimal results. Always consult with your eye care provider to determine if RF therapy is the right treatment option for you.
Thermal Pulsation is a therapy in which the eyelids are heated and massaged to unclog oil glands. While this treatment is effective to relieve symptoms, we do not currently offer it as an option, as it does not treat the underlying cause. WHY are the oil glands clogged? Are they clogged because of low omega levels? Hormone imbalances? Rosacea, demodex mites, bacterial infections, poor blink, inflammation... We treat the underlying cause, not the symptom.
We do not discount the fact that many patients feel a benefit from this treatment and will recommend an office who offers this procedure if we feel it would benefit you.

READY FOR THE NEXT STEPS?
Don't Delay Feeling and Seeing Better. Begin Your Journey Today!


